REHOVOT, ISRAEL—May 19, 2021—Our livers work hard to perform a significant range of activities: helping us digest food, maintaining body temperature, and serving as an important checkpoint of the immune system for everything that we eat. It is inside the liver that the unique, rich, and complex network of immune cells and pathways is set up to decide whether a food particle is harmless or a dangerous pathogen that should be neutralized and removed. The liver is, therefore, very sensitive to the food we consume, and sometimes a poor diet can induce a serious dysregulation of the immune activities within it.
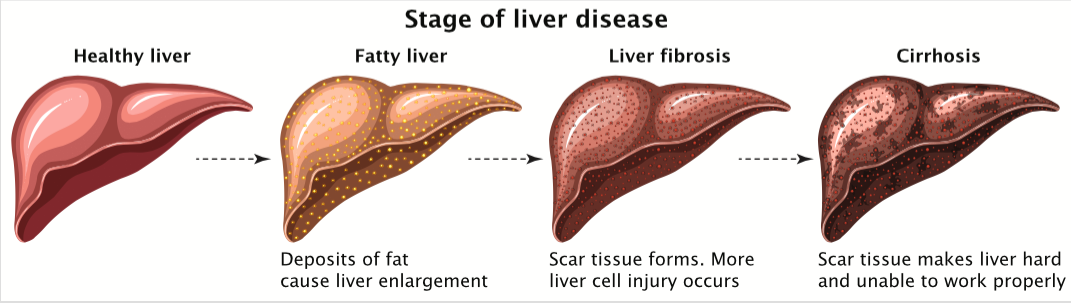
Obesity is an extremely prevalent condition in the Western world, and 90 percent of people with obesity also show signs of fatty liver. This condition is harmless in itself, accompanied by no special symptoms – although presenting with aberrant liver metabolism – and resolves by itself upon weight loss. However, if patients maintain their unhealthy habits (high caloric food intake, sedentary lifestyle), at least 20 percent of them will develop a condition involving liver-cell death and inflammation called non-alcoholic steato-hepatitis (NASH), which can lead to liver fibrosis, life-threatening cirrhosis, and liver cancer.
In a recent study reported in Nature Medicine, the Weizmann Institute of Science’s Prof. Ido Amit and team members Dr. Aleksandra Deczkowska, Eyal David, and Dr. Assaf Weiner and Prof. Eran Elinav’s laboratory, in collaboration with the Center for Liver Diseases at the Chaim Sheba Medical Center (Tel Hashomer) and Prof. Mathias Heikenwaelder’s laboratory at the German Cancer Research Center (DKFZ), investigated the relationship between the liver’s immune system composition and NASH pathology. They discovered that dendritic cells – a subtype of immune cells – become activated in the liver in NASH patients and in animal models, and promote the condition’s progression. This finding may, in the future, help develop new treatments for NASH.
In order to study the immune system in NASH, the scientists kept laboratory mice on a diet similar to an unhealthy human diet – lacking in essential nutrients and enriched with fat- and cholesterol-laden “junk food” – and monitored the condition’s development. To survey the global immune changes in the immune cells in the liver, the researchers used a new technology they developed for single-cell RNA sequencing, which enables an unbiased analysis of tens of thousands of single cells without making any assumptions about their identities. Using this technology, the scientists found that, in NASH, a subtype of dendritic cells called type 1, or cDC1, greatly expands. To make sure that this phenomenon is related to liver disease and not to a particular diet, the researchers used six different models of obesity and unhealthy metabolic diet – and found that the cDC1 count was always elevated when NASH was induced.
To determine whether this phenomenon is unique to animal models or is also relevant to human NASH, the researchers examined liver tissue biopsied from patients on the spectrum between non-alcoholic fatty liver disease and NASH, and found that numbers of cDC1 correlated with the extent of liver pathology: the more the cDC1 counts were elevated, the greater the liver damage. Interestingly, cDC1 cells were also found in higher numbers in the blood of patients with fatty liver and NASH, suggesting that NASH may alter the course of hematopoiesis – the process of blood cell production in the bone marrow – by skewing it towards increased production of dendritic cells, but not other blood cells. Indeed, in the bone marrow of mice with NASH, the immature progenitor cells that give rise to dendritic cells were indeed found to be proliferating at a higher intensity.

At this point, the researchers asked: What is the role of the cDC1s in NASH? And if we manipulate them, what would be the effect on liver pathology? To answer these questions, they used two independent approaches to remove the cDC1s from the system while inducing NASH, then measured the consequences of cDC1 absence. In one approach, mice were genetically engineered to lack cDC1s; in the other, cDC1 infiltration to the liver was blocked using targeted therapeutic antibodies. In both cases, lowering the numbers of cDC1s correlated with an alleviation of disease pathology. Especially in mice treated with cDC1 blockers, signs of severe liver damage in the blood – assessed by blood tests – were lowered after treatment.
What is the mechanism behind these effects?
In a normal immune response scenario, dendritic cells, which are the immune system’s primary “CPU,” scan organs looking for immune cues, then travel to organ-linked lymph nodes – the immune response command centers – to communicate this information to T cells. The T cells then issue instructions to other cells involved in immune responses. The scientists hypothesized that this communication pathway is important in NASH, because the cDC1s are known to specifically interact with a subtype of T cells called CD8+, which – as the scientists had shown in another collaborative study published in Nature – promote NASH and NASH-related liver cancer.
To check whether the cDC1s indeed instruct the CD8+ cells to promote liver damage, the scientists isolated pairs of physically interacting cDC1 and T cells from mice with and without NASH. They found that in NASH, the cDC1s lead to induction of liver damage-inducing T cells that are more aggressive and inflammatory.
Overall, the cDC1s seem to be an important player in NASH. Manipulating this cell type may in the future be considered a therapeutic way of dealing with NASH and its severe consequences.
Lead author Dr. Aleksandra Deczkowska explains: “We know that the immune system has a role in protecting us from pathogens, but in recent years, it has been found to be involved in other diseases, including cancer, obesity, diabetes, or even Alzheimer’s. The healing potential of the immune system can be harnessed for treating these diseases, instead of targeting the disease mechanisms directly. This approach, known as immunotherapy, has already led to recent breakthroughs in cancer treatment, and we believe it will soon be extended to other medical problems, such as NASH.”
Prof. Ido Amit is the incumbent of the Eden and Steven Romick Professorial Chair. His research is supported by the Helen and Martin Kimmel Award for Innovative Investigation; the Moross Integrated Cancer Center; the Belle S. and Irving E. Meller Center for the Biology of Aging; the Joel and Mady Dukler Fund for Cancer Research; the Thompson Family Foundation Alzheimer’s Disease Research Fund; the Adelis Foundation; Richard & Jacqui Scheinberg and the Garvan Weizmann Partnership donors; the Ben B. and Joyce E. Eisenberg Foundation; the Wolfson Family Charitable Trust and the Wolfson Foundation; the Vainboim Family; and Miel de Botton.
Prof. Eran Elinav is the incumbent of the Sir Marc and Lady Tania Feldmann Professorial Chair of Immunology. His research is supported by the Belle S. and Irving E. Meller Center for the Biology of Aging; the Jeanne and Joseph Nissim Center for Life Sciences Research; the Swiss Society Institute for Cancer Prevention Research; the Norman E Alexander Family M Foundation; the Coronavirus Research Fund; the Leona M. and Harry B. Helmsley Charitable Trust; the Mike and Valeria Rosenbloom Foundation; the Isidore and Penny Myers Foundation; the Adelis Foundation; the Ben B. and Joyce E. Eisenberg Foundation; Miel de Botton; the Vainboim Family; and the European Research Council.
