Everyone experiences anxiety at times, but for some people, it’s a pervasive condition that can turn the ordinary into the distressing. The National Institute of Mental Health reports that 1 of every 10 women and 4 of every 100 men will suffer from post-traumatic stress disorder (PTSD) at some time in their lives – for example, as a result of trauma experienced in war or from all-too-common events such as accidents, crime, or sudden health conditions. Even more people suffer from generalized anxiety without a specific memory of an experience they can point to as a cause.
But even if we understand that trauma can lead to neuropsychiatric conditions – debilitating stress, PTSD, anxiety, major depression – how, exactly, do such experiences affect the brain and result in long-term anxiety?
Prof. Rony Paz of the Weizmann Institute of Science’s Department of Neurobiology is finding the answers.
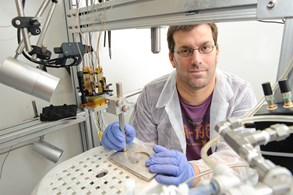
Prof. Rony Paz
Curious about the brain’s fear- and anxiety-related circuitry, Prof. Paz is particularly interested in discovering how anxious people perceive the world and how PTSD develops. For example, PTSD occurs in only some of the population, and the differences between people who develop it and those who don’t “are not just genetic, as current thinking would have it,” says Prof. Paz, “but are rooted in the exact way in which each memory was formed.”
Two very different parts of the brain, the amygdala and the prefrontal cortex, are certainly involved. The almond-shaped amygdala plays a crucial role in regulating emotions and in forming emotion-laden memories. The prefrontal cortex helps control learning and logical, rational thinking. The delicate, precise balance between the two systems is crucial for normal daily function,and problems with the connection between the amygdala and the prefrontal cortex can result in neuropsychiatric illnesses such as autism, depression, and anxiety disorders.
Prof. Paz hopes that unraveling the relationship between these two vital parts of the brain will shed light on anxiety and PTSD, allowing him to find more effective ways to help sufferers. “In order to devise better treatments, we need to be able to understand exactly where and how, in a particular individual, these two brain networks are out of balance,” he says.
“Our vision is that we’ll be able to help inhibit the memory of a specific traumatic event – and only that event.”
His investigations suggest that development of PTSD may be tied to the context in which disturbing memories are formed. For instance, the element of surprise makes a memory more resistant to change, and thus more likely to become traumatic and resist therapy. This helps explain why soldiers in a war zone, where attacks can – and do – take place at any moment, are more likely to develop the disorder. It has been shown that the incidence of PTSD also increases after soldiers transfer to a new, unfamiliar unit.
But how do these resistant memories gain their foothold in the brain? Prof. Paz found that their formation involves a dialogue between the amygdala and an area of the frontal cortex called the anterior cingulate cortex (ACC). The level of coordination between these parts of the brain can be used to accurately predict how strongly a memory will be held, leading Prof. Paz and his team to see if they could interfere with the way traumatic memories are stored.
Using a method known as deep brain stimulation (DBS), they suppressed ACC activity in an animal model. A control group did not receive the treatment. “Traumatic memories” were then induced in both groups by playing a specific tone that was followed by an extremely bad smell. The next day, the control animals displayed obvious signs of distress upon hearing the tone, while those that had been treated with DBS had a much milder response. In fact, the more effective the DBS (and the more suppressed the ACC activity), the calmer the animals were – even three days later.
A second mechanism found by Prof. Paz’s lab shows that people suffering from anxiety may have a tendency to lump together similar sensory stimuli. As an example, many who witnessed the 9/11 terror attacks in New York City developed PTSD, which could be triggered by just the sight of a tall building. “If a person with PTSD encounters a stimulus that is even remotely similar to the original one that caused anxiety,” he says, “their brain may ‘overgeneralize’ and produce fears.”
This overgeneralization, he recently found, is a trait common to the anxious person; in fact, such people literally perceive the world differently. In experiments, anxious subjects responded emotionally to new, neutral stimuli as well as to previously upsetting stimuli, exhibiting “anxiety symptoms even in apparently irrelevant situations,” Prof. Paz says. “They cannot control this response: it is a perceptual inability to discriminate.”
Anxious people can overgeneralize, experiencing “anxiety symptoms even in apparently irrelevant situations,” says Prof. Paz. “They cannot control this response.”
Prof. Paz explains that this blurring of perceptions likely helped our ancestors survive. As he put it, “If the best response to the growl of a lion is to run quickly, it would be counterproductive to distinguish between different pitches of growl.” But in today’s sensory jungle, that tendency could make any loud noise evoke the same gut reaction as, say, gunfire.
As a pioneer in the new field of interdisciplinary neuroscience, Prof. Paz combines computational and physiological approaches to brain studies. Because the brain is such a complex organ and neuropsychological conditions are a result of complicated computations occurring in this system, such an approach must be taken in order to understand the causes of – and develop means to help people with – severe anxiety, PTSD, depression, and other neuropsychological conditions.
This approach also makes him a natural fit for the Weizmann Institute, with its emphasis on multidisciplinary research. A native Israeli, Prof. Paz returned home and joined the Institute in 2007, after a prestigious Fulbright fellowship took him to Rutgers in New Jersey for postdoctoral research. Today, he is uniting machine learning with behaviorism, statistics with cognitive psychology, computer science and math with biology and neuroscience – all with stunning results.
It is this blending of methods that could change lives. “In the future, I believe it will be possible to treat and diagnose PTSD with a combination of physiological manipulations and behavioral therapy,” says Prof. Paz. “Our vision is that we’ll be able to help inhibit the memory of a specific traumatic event – and only that event. The combined approach – computational, physiological, and behavioral – would avoid the psychological and physiological side effects of today’s drug-based therapies, and treat the core of the problem itself.”
The research of Prof. Rony Paz is supported by the Adelis Foundation; the Sylvia Schaefer Alzheimer’s Research Fund; the Irving and Dorothy Rom Family Discovery Endowment Fund; Pascal and Ilana Mantoux, Israel/France; the Minna-James-Heineman Stiftung; and Gary and Kary Leff, Calabasas, CA.
