Identifying who is most at risk for a deadly cancer
Lung cancer is one of the deadliest cancers, primarily because it is rarely diagnosed in its early stages. Lung cancer is largely preventable, since 90 percent is caused by smoking. Yet only 10 to 15 percent of heavy smokers develop lung cancer, and these odds give many smokers a false sense of security.
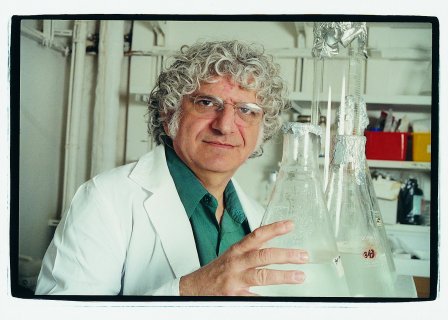
Prof. Zvi Livneh and his team of Weizmann Institute scientists in the Department of Biological Chemistry have pinpointed an enzyme that plays a role in protecting individuals against lung cancer. Genetic differences in the activity of this enzyme may help explain why some get cancer and others don't. The scientists hope the finding will be used to assess a smoker's risk for lung cancer, making it easier to persuade high-risk smokers to kick the habit.
How cancer occurs
When we are young and growing, many of our body's cells multiply constantly. After we reach maturity, cells begin to multiply for replacement only, rather than growth; they are programmed to know when to stop. Cancer occurs when cells lose their "brakes" and multiply in an uncontrolled fashion.
"Cancer means a genetic change (mutation) has occurred. You must control mutations to prevent cancer or slow its progression. This requires an understanding of what makes a normal cell suddenly transform into a cancer cell," Prof. Livneh told an audience in Florida.
Human DNA is comprised of information bits that are chemically coded T,C,G, and A. DNA is formed in two long strands that are twisted together in a double helix pattern. When a cell multiplies, the DNA strands separate, and each strand then makes a copy to form a new double helix. The replication process is highly accurate, but not perfect: each cell averages 1 "typo" in 10 billion letters. These mistakes are greatly increased by external DNA-damaging agents, such as sun, tobacco smoke, or food additives, or internal processes, such as waste products left over from the body's own metabolic processes.
"There is no way to avoid damage. It's a part of normal life," said Prof. Livneh.
When DNA damage is extensive, a cell might choose to commit suicide. Cells, however, prefer to continue replicating. To this end, sophisticated DNA repair mechanisms in the cell recognize damage, cut short segments out of the strand, and replace the damaged bits. Countless instances of damage are caught and repaired daily. Yet some escape proper repair. The replaced segment might contain mismatched letters, for example. If the mutation is passed on unrepaired, it can eventually lead to cancer. Five to 20 mutations must accumulate in a single cell before it begins to divide in an out-of-control fashion.
Finding a way to measure DNA repair
"Cancer can be caused by the excessive actions of DNA-damaging agents such as tobacco smoke or other external factors, the reduced ability to respond to this damage with DNA repair mechanisms or, more likely, a combination of both," said Prof. Livneh. "We know this because as our ability to repair DNA decreases, cancer risk rises."
Prof. Livneh and his colleagues have identified an enzyme, known as OGG1, which plays a central role in repairing a type of DNA damage that can lead to lung cancer and head and neck cancers.
High levels of OGG1 are desirable — nonsmokers have an average OGG1 level of 7. Smokers with an OGG1 level of 4 have 124 times the risk of lung cancer than nonsmokers with normal OGG1 levels. (A high level, of course, is not a 100 percent guarantee that cancer will not develop, nor does it protect against other effects of smoking such as hypertension.)
The goal
Applying this information to medicine requires only the development of a simple blood test for OGG1 levels. "The test could be used to screen smokers. It might be a convincing tool to warn those most at risk to stop smoking. If you have low OGG1 levels, you should reduce your exposure to tobacco, ultraviolet radiation, and other carcinogens," said Prof. Livneh. "It would also open the door to developing drugs to strengthen OGG1 levels."
While knowing the role of OGG1 cannot, at present, prevent cancer or stop mutations from occurring, it might help those at risk postpone the development of cancer until it becomes irrelevant. "Since the incidence of cancer increases with age, if you reduce the rate at which mutations accumulate, you can delay the age at which cancer appears. Who cares if you get cancer when you are 120?" Prof. Livneh said.
Prof. Zvi Livneh's research is supported by the M.D. Moross Institute for Cancer Research; the Dr. Josef Cohn Minerva Center for Biomembrane Research; the J & R Center for Scientific Research; and the Levine Institute of Applied Science. Prof. Livneh is the incumbent of the Maxwell Ellis Chair of Biomedical Research. The Weizmann Institute of Science in Rehovot, Israel, is one of the world's foremost centers of scientific research and graduate study. The American Committee for the Weizmann Institute of Science is a community of dedicated people who share a common vision in support of the Institute. The generous assistance the Weizmann Institute receives from individuals, foundations, and corporations is vital for its future. Committee members show their devotion to the advancement of the Institute's goals by becoming partners in the search for answers to the most difficult challenges facing humanity.
